
FACT: The Netherland’s Flexible Assertive Community Treatment for mental illness (2003 – ongoing)
Facing rising suicide rates and increasing numbers of individuals with lived experience of mental health challenges, the Dutch government has made an effort to introduce a more flexible mental healthcare model. Flexible Assertive Community Treatment (FACT) is an innovative, integrated care model, based on the Assertive Community Treatment model from the US. It seeks to shift the focus of treatment from the clinic to the community, with the goal of improving continuity of care.
The assertive outreach component has proved to be particularly effective in averting relapses, rehospitalisations and other crises, because its modus operandi offers flexible reevaluation of the risk assessment of patients.[1] Although evidence about FACT‘s effectiveness has been mixed, it has been successful in integrating different services within the Dutch mental healthcare sector, while also being cost-effective.
The initiative
Two Dutch healthcare professionals - Michiel Bähler, a psychologist, and Remmers van Veldhuizen, a psychiatrist - jointly developed the FACT mental healthcare model, which was launched in 2003 in the Noord-Holland province of the Netherlands. GGZ Nederland, the Dutch Association of Mental Health and Addiction Care, is the sector organisation of specialist providers that has been responsible for the design and implementation of FACT in the Netherlands. It has been expanded across the country, and there are currently about 200 expert teams around the country. In some areas, the model has been fully implemented, and an expansion to 400-500 FACT teams is predicted over the next few years.[2]
In the Netherlands, FACT is a broad “biopsychosocial model”, providing: management of illness and symptoms (i.e. “treatment”); guidance and practical assistance with daily living; rehabilitation; and recovery support. An integrated multidisciplinary FACT team of 11-12 fulltime experts monitors 200 clients in a particular district or region of 40,000 to 50,000 inhabitants.[2] The team tries to establish close contacts with the family and with other services in the district. The team is multidisciplinary, with members from a wide variety of disciplines, including a psychiatrist, a community psychiatric nurse, other nurses, a psychologist, an employment specialist, an addiction specialist, and a peer support worker.[2]
The target group is formed of individuals with lived experience of mental health conditions in a particular catchment area, both the 20 percent for whom ACT is indicated and the remaining 80 percent, who need less intensive treatment and support. To combine care for these two groups, the FACT team employs a flexible switching system. The multidisciplinary team can switch back and forth between two modes of care delivery: individual case management by a member of the team, and intensive ACT team care. The latter model involves clients having contact with several team members. The clients requiring the most intensive care are listed on the FACT board, which is an Excel spreadsheet beamed on to the wall. The team adopts a shared caseload approach and discusses the intensive care patients every day to decide which form of care should be provided and by which team members.
For clients requiring less intensive care, the same team provides individual case management with multidisciplinary treatment and support. When clients become more stable, they do not have to be transferred to a different team; they stay with the same FACT team. This flexibility to switch between the two modes of service delivery in the same team enhances continuity of care and reduces dropout rates, while also being the response needed for the natural course of severe mental conditions, with the customary remissions and relapses.[2]
FACT has been shown to improve recovery prospects and support during recovery and rehabilitation periods. As soon as a client is at risk of their illness recurring, potentially resulting in hospitalisation, the same team switches to intensive ACT. [2]
FACT teams are also starting in Belgium, and mental healthcare practitioners and organisations in Hong Kong, Norway, Sweden and the UK are looking into the possibilities of integrating the principles of FACT into their existing systems.[2]
The challenge
In the Netherlands, there has been a challenge to develop a model of mental healthcare that would better meet the needs of individuals experiencing challenges to their mental health and support community-based recovery and social inclusion. Policymakers sought to develop a model that would support the integration of community and hospital care and incorporate evidence-based medicine and best practices.[2]
Rising suicide rates and high rates of depression have adversely affected the Netherlands. Mental disorders are responsible for high productivity losses, amounting to 12 million sick days annually at a cost of EUR2.7 billion. Depression has been the greatest burden of all health conditions, affecting 8.2 percent of Dutch people in 2011, greater than cardiovascular disease or cancer. FACT's founders estimate that out of the “population of nearly 17 million, there are 162,000 people aged between 18 and 65 with severe mental illness”.[2] This is despite the fact that the cost of treating depression for the whole population is comparatively small, at approximately 1 percent of the national healthcare budget.[3]
The Dutch mental healthcare system remains largely hospital-based. In comparison with other countries, the duration of admissions is still long, sometimes very long. Internationally, along with Belgium, and to some extent with Germany, the Netherlands has the highest number of psychiatric beds per capita in the world - more than twice as many as the UK and four times as many as Australia.
In contrast with other European countries, the US, and Australia, there has been only a moderate degree of deinstitutionalisation in the healthcare sector. In 2005, there were still 12,000 long-stay beds in the country. Long-stay wards have been downsized slowly over the last 20 years, and in 2011 it was agreed that 30 percent of the capacity would be phased out within 10 years.[2] However, the needs of long-term patients in the community grew more rapidly than could be met by downsizing the wards.[1]
The system failed to provide the necessary support for those experiencing mental health challenges that live in the community. In addition to these challenges, they can also find elements of social functioning challenging, such as those relating to housing, self-care, employment and finances. It is often difficult for them to participate in society and feel a sense of belonging. “Their support systems and contacts are often limited. Family is very important, but sometimes family is kept at a distance.”[2]
Until 2002, community support was provided by case management teams. In some cases, the psychiatrist was a member of the team, but in other cases the teams had to link people to psychiatrists working elsewhere in the service. The transmural care system already ensured 24-hour crisis service coverage and continuity of care in the event of hospitalisation. This system worked for many people, but if they became unstable and needed more support than once or twice a week, the case managers ran into problems with their caseload. As a result, too many people were readmitted too frequently, and others could not be discharged from hospital.[1]
One solution proposed was ACT, which was developed in the 1970s in the US. However, ACT only focuses on 20 percent of the most severe cases of mental illness and leaves out many people who require care and hence causes discontinuity of care between acutely ill and currently stable patient groups.
The public impact
Many studies suggest that FACT has had a positive impact on the quality of mental health services and is cost-effective, but more evidence-based policy evaluation is required to assess its impact more precisely. One study, conducted between 2005 and 2013, has shown that the remission of schizophrenia increased from 19 percent in the period before the introduction of FACT to 31 percent during the period after its introduction. Hospital bed usage and admission rates were reduced, and patients‘ quality of life was increased.[4]
In a recent evaluation of the policy, the number of admissions, admission days, and face-to-face contacts differed between ACT and non-ACT patients, but in general they decreased. The evaluation‘s findings also suggested that implementation of FACT has resulted in a more flexible adaptation of care to patients‘ needs.[5] On the other hand, some researchers have warned that the FACT model, which provides both intensive and less intensive care, is not beneficial for intensive care patients, because other patient groups may "dilute" care provision.[6]
While FACT care is relatively expensive, it clearly generates some medical, social and economic benefits. A recent study from 2018 on the cost-effectiveness of the transition to community-based healthcare shows that, for the group of patients who were treated under FACT, the cost of treatment was reduced by an average of EUR2,132, with similar health outcomes as in the old, hospital-based system.[4]
In addition, clients, family and partners are positive about FACT. It helps address issues of nuisance and neglect, more people with severe mental illnesses have a chance to obtain paid work, and the number of hospital beds can be reduced. "After 2 years it became clear that at any one point not 20 percent but only 10-15 percent of patients needed to be put on the whiteboard for ACT service with assertive outreach and shared caseload. After the FACT teams were set up, we saw a gradual decrease in admission days and an increase in admissions."[1]
Stakeholder engagement
There has been strong engagement between psychiatrists and psychologists - some of whom were involved in developing FACT - and GGZ Nederland (the Dutch Association of Mental Health and Addiction Care), which is the government organisation responsible for FACT‘s design and implementation. GGZ Nederland has more than 100 member organisations and is the country's professional body for specialist mental health and addiction care providers.[7]
Through this network, GGZ Nederland has been able to transform the practitioners' vision into an active policy. Its member organisations deliver a wide range of services to the public, ranging from mental health promotion and prevention and primary mental healthcare to assisted independent living, sheltered housing, ambulatory specialist mental healthcare, clinical psychiatric care, and forensic institutional care.[7] The initiative has been supported by other stakeholders, including peer support workers, GPs, nurses, employment rehabilitation specialists, and governmental bodies such as the Ministry of Health, the Dutch Association of Mental Health, and local governments.
Political commitment
Dutch politicians have strongly supported FACT, due in part to their dissatisfaction with the institutional model of care, which has a record of mistreatment and abuse of psychiatric patients. In 1994, parliament passed the Psychiatric Hospitals Compulsory Admission Act, in reaction to the often paternalistic and abusive Dutch psychiatric institutions of the 1950s and 1960s. The thresholds for voluntary and involuntary admission were raised. Patients committed to hospital could be treated against their will only in the event of "severe danger in the hospital".
However, problems related to people experiencing serious challenges to their mental health grew much more rapidly than the solutions. And by the turn of the century, this whole situation had led to what could be termed a paralysis of care. A growing sense of urgency for change coincided with a spate of international publications about ACT, which seemed to offer a viable solution for the Netherlands.
Public confidence
Since FACT teams now operate throughout the Netherlands, acceptance of and public support for FACT's working procedure has been growing, especially among clients' families. More and more family members have heard about it, and are much less critical than they were around 2005, when FACT was sometimes seen as a “potential disruption of a patient's safe existence in an institution”.[2]
At first, family members were surprised by the change to home visits. Sometimes, clients did not like the fact that several different team members came to see them instead of a single contact coming to see them regularly. It proved helpful to explain why this was done: that only a team can provide intensive care; that if the client's own case manager is ill or on holiday, treatment can continue as usual; and that, in the long run, it can be more pleasant for clients to have contact with several people rather than one. Now, patients' and families' organisations strongly support the FACT model, and FACT's rapid expansion and implementation is partly due to this support.
To build on this growing public confidence and participation in the initiative, the F-ACT Nederland association set up an expertise platform where clinicians, mental healthcare practitioners, and patients could share treatment insights about FACT.[8]
Clarity of objectives
FACT has clearly defined objectives that have been maintained throughout its implementation. When the FACT teams began operation, this led to a rethinking of the broader mental healthcare system. The Certification Centre for ACT & FACT (CCAF) developed the FACT model with the broad aims of combining:
- Recovery-oriented care
- Evidence-based medicine and best practices
- Integrated community and hospital care
The main goal is to “ensure continuity of care, to prevent admissions to psychiatric hospitals and to stimulate inclusion, so that clients can participate in society”, as stated in the manual accompanying the policy.[2] This goal has been maintained throughout the policy, while a further approach for clients - the “self-reliance” approach - has been introduced. It allows clients, with the support of care workers, to set new goals in relation to their environment and work on tasks they themselves have formulated.[2]
Strength of evidence
The Dutch FACT system is a development and extension of ACT, which was introduced in the 1970s in the US and has been widely acclaimed and proved highly effective since then.[1] Within the ACT framework, a multidisciplinary team consisting of 11-12 fulltime experts cares for around 100 clients with a shared caseload, so that all the members of the team know all the clients. The approach focuses on outreach and on providing persistent and very intensive care and treatment for the most severely challenged 20 percent of persons in the community, particularly for hard-to-engage persons who are at risk of hospitalisation, homelessness or neglect.[2] Other key characteristics of ACT include home-based treatment and out-of-hours availability. In addition, ACT provides integrated dual diagnosis treatment, supports paid employment, and incorporates peer support.[1]
Further evidence was gathered through implementing FACT in three pilot programmes in the Dutch province of Noord-Holland, a region in which a cumulative routine outcome measurement system was in place to serve all the long-term psychiatric patients living in the community.[1] It was run by GGZ Noord-Holland, based in Alkmaar. "Patients receiving FACT were compared with patients receiving standard treatment, matched on ‘baseline' symptom severity and age, using propensity score matching. The outcome was the probability of being in symptomatic remission of psychotic symptoms."[6]
The FACT model was, then, first implemented in four teams in a region with 225,000 inhabitants.[1] Based on this real-life experience, the model was developed further. When the pilot team phase came to an end, a seminar was held for families, municipal authorities, and other mental healthcare organisations involved in the care, so that everyone was involved in the transition to the new model of care delivery.[2] In the course of implementation, broad impact research had been carried out and fidelity scales had been developed. The FACT fidelity scales are used to qualitatively assess care circuits on a number of criteria, including its team structure, domains of care, its case mix and resources through a rating system.[12]
Feasibility
Funding for FACT comes partly from private insurers and partly from the government (shared between the federal government and the municipalities). These funding bodies make arrangements with local mental healthcare providers in 20 to 30 different regions of the country. The use of the FACT model has helped to clarify the complex arrangements between so many different parties.[2] Even though FACT is relatively expensive compared to conventional treatment methods,[2] because it involves more personnel than a general admission to hospital does, Dutch mental health services have been relatively well funded throughout the implementation of FACT, and the availability of these services has been ensured since its introduction.
The ability of outpatient and inpatient care providers to coordinate the delivery of mental health services successfully is another indication of the model's feasibility. When inpatient care is no longer required, members of FACT teams visit their clients at the clinic every week. They are involved in discussions of treatment plans. The team makes clear and detailed arrangements regarding these matters with a psychiatric unit in the area. Many mental health service organisations arrange for the FACT psychiatrists and the hospital psychiatrists to meet once a week to discuss and coordinate treatment. However consultations with psychiatrists and psychologists may not comply with the rule that the location of FACT should be in the neighbourhood where the team works; often, FACT teams can be located a significant distance from their neighbourhoods.[2]
Management
FACT's management system is one of its principal strengths. It allows for a high degree of coordination of care and collaboration with other services, including the hospital system.
FACT teams are district-based and provide care for all individuals with severe mental illness in a particular neighbourhood or district of approximately 40,000-50,000 inhabitants. This localised approach facilitates collaboration with other social services and with GPs. They operate in accordance with the typically Dutch model of "transmural care". The FACT team is not only a gatekeeper for the hospital but also stays in touch with the client during their admission and retains the overall coordination of the client's treatment.[2]
The names of clients receiving intensive team care are listed on the FACT whiteboard (see the Initiative above). Every morning, the team meets to discuss the FACT board and decide which team members will visit and supervise the clients. At least once a year, the multidisciplinary team discusses each client's treatment plan with them, including crisis and rehabilitation plans, using up-to-date information from the Health of the Nation Outcome Scales (HONOS), an observational list scale that assesses a patient's mental health. The HoNOS scales contain 12 items measuring behaviour, impairment, symptoms and social functioning. The scales are completed after routine clinical assessments in any setting.
Clients receiving individual support are not listed on the FACT board. They always have their own case manager and psychiatrist. Other team members can be called upon for specific components of treatment or support, for instance, the addiction specialist or a psychologist for Cognitive Behavioural Therapy.
FACT teams work during office hours and some teams also visit clients at home during weekends. Every region in the Netherlands has a readily accessible psychiatric emergency service, available 24/7. FACT teams work in close conjunction with regional inpatient clinics.[2] Each team has to be certified by CCAF, a special certification centre which has already certified more than 300 teams.[9] CCAF also provides training courses for the pilot teams, as well as later on for the other teams seeking to introduce and improve everyday working procedures. Most training courses focus on the change in attitude required between working in an inpatient or outpatient clinic and working in outreach care.[2]
Measurement
Model fidelity and clinical and social assessments were performed at baseline in 2003 and after one and two years internally by CCAF. To assess the implementation of the FACT model, in 2007 CCAF published a FACT scale. The scale assesses the ability of FACT teams to deliver optimal community treatment, the ability to scale care up and down flexibly, and the quality of treatment across the whole continuum of care, from GP and district social services to inpatient care.[2]
During the first two years, this fidelity scale has been used to rate around 70 FACT teams, while others followed in subsequent years. In response to the outcomes and experiences of the teams assessed so far, the scale was adapted in 2013 and has since certified almost 300 teams. Every one to two years, CCAF sends two assessors, who are also practitioners, to monitor the team's meetings, file-keeping, and general working procedures. The team's ongoing certification is determined by this assessment.
CCAF is now widely known and recognised in the Netherlands. Insurers and funding bodies require mental health organisations to have their teams certified according to CCAF's requirements. Countries like Belgium and Sweden have expressed their interest in adopting a similar kind of certification for their mental healthcare teams, and in Sweden, the first international assessment of a team in Gothenburg has begun.[2]
External studies of FACT's effectiveness have identified some methodological limitations. The primary outcome measured in academic studies was the symptomatic remission of psychotic disorder. A review of seven studies assessing FACT's impact suggests that all seven lacked a precise definition of “remission”, and it concludes that it cannot convincingly be shown that FACT leads to an improvement in clients' symptoms, functioning or wellbeing. "Furthermore, it is not clear which patients who were truly in remission, given that the criteria from the international remission working group were not followed."[10]
Alignment
FACT is part of a community support system that comprises multiple agencies with a common goal of support and social inclusion of people with lived experience of mental health conditions. However, this alignment is compromised by a lack of organisation, consistency, and accessibility among the various community and welfare services.
Another difficulty for practitioners is to work with a shared caseload; formerly, Dutch healthcare specialists had been trained to work individually and were unfamiliar with sharing their patients with external practitioners. The idea of team care is sometimes resisted by individual care practitioners.[2]
In 2018, the European Commission published a guide on mental health practices for the EU and assessed the Dutch FACT model.[11] Regarding the alignment of the actors responsible for the policy's success, it found two main impediments to the alignment of stakeholders:
- "The mental health services stakeholders from community mental health teams and the psychiatric hospitals belonged to different work and care cultures with different visions
- "In the financial structure of mental health services, there were financial incentives that support hospitalisation. Therefore, the transition of hospital based to community-based mental health care with FACT teams was a financial risk for the mental health services involved."[11] Hospitals, in particular, were initially reluctant to push for a switch from inpatient care to outpatient care.
There exists the possibility of future fragmentation of the Dutch mental healthcare system, which could impact on FACT because it will create a more complex network of stakeholders and make stakeholder alignment a more difficult prospect. Until now, the entire mental healthcare system has been financed under a single piece of legislation. However, changes in other healthcare sectors, such as nursing homes and general hospitals, as well as rising expenditure on healthcare as a whole, have led the Dutch government to introduce a new financial system, which will be implemented during the coming years.
Consequently, many components of the service that FACT teams provide will be financed from several different sources and under different legislation. Insurance companies, municipalities, and possibly the minister of justice will be the new financial stakeholders. This poses a real threat of future fragmentation of FACT and other psychiatric services, according to a study conducted by Dutch researchers.[1]
Bibliography
[1] FACT - A Dutch Version of ACT, Remmers van Veldhuizen, Community Mental Health Journal, 2007
https://link.springer.com/article/10.1007/s10597-007-9089-4, last accessed 24 August 2019
[2] Manual: Flexible Assertive Community Treatment, Remmers van Veldhuizen and Michiel Bähler, 2013, CCAF
https://www.eaof.org/factmanual.pdf, last accessed 25 August 2019
[3] The Netherlands has an innovative mental health system, but high bed numbers remain a concern, February 2000, OECD Mental Health Policy,
https://www.oecd.org/els/health-systems/MMHC-Country-Press-Note-Netherlands.pdf, last accessed 24 August 2019
[4] Doing more than ACT: The Dutch FACT model, flexible assertive community treatment, René Keet, March 2016, European Psychiatry https://www.sciencedirect.com/science/article/pii/S0924933816017697, last accessed 23 August 2019
[5] Outcomes of FLEXIBLE Assertive Community Treatment (FACT) Implementation: A Prospective Real Life Study, M. Annet Nugter, Fabiana Engelsbel, Michiel Bähler, René Keet and Remmers van Veldhuizen, 2016, Community Mental Health Journal
https://link.springer.com/content/pdf/10.1007%2Fs10597-015-9831-2.pdf, last accessed 20 August 2019
[6] A real-life observational study of the effectiveness of FACT in a Dutch mental health region, Marjan Drukker et al, 2008, BMC Psychiatry, https://bmcpsychiatry.biomedcentral.com/track/pdf/10.1186/1471-244X-8-93, last accessed 29 August 2019
[7] Dutch Association of Mental Health and Addiction Care, GGZ Nederland,
https://www.ggznederland.nl/pagina/english, last accessed 28 August 2019
[8] F-ACT experience expertise, F-ACT Nederland,
https://www.f-actnederland.nl/ervaringsdeskundigheid/, last accessed 27 August 2019
[9] CCAF, Centre for Certification FACT & ACT,
https://ccaf.nl/, last accessed 27 August 2019
[10] Absence of Positive Results for Flexible Assertive Community Treatment: What is the next Approach? Tommy Nordén and Torsten Norlander, 2019, Journal of Clinical Practice & Epidemiology in Mental Health,
https://benthamopen.com/FULLTEXT/CPEMH-10-87, last accessed 27 August 2019
[11] Good Practices in Mental Health and Wellbeing: Mental Health Services in the Community, 2018, Consumers, Health, Agriculture and Food Executive Agency (Chafea), the European Commission,
[12] FACT Fidelity Scales 2017, CCAF Workbook, Bähler et al. (2017), Utrecht, https://ccaf.nl/wp-content/uploads/sites/2/2017/11/FACT-Fidelity-Scale-2017.pdf, last accessed 11 September 2019
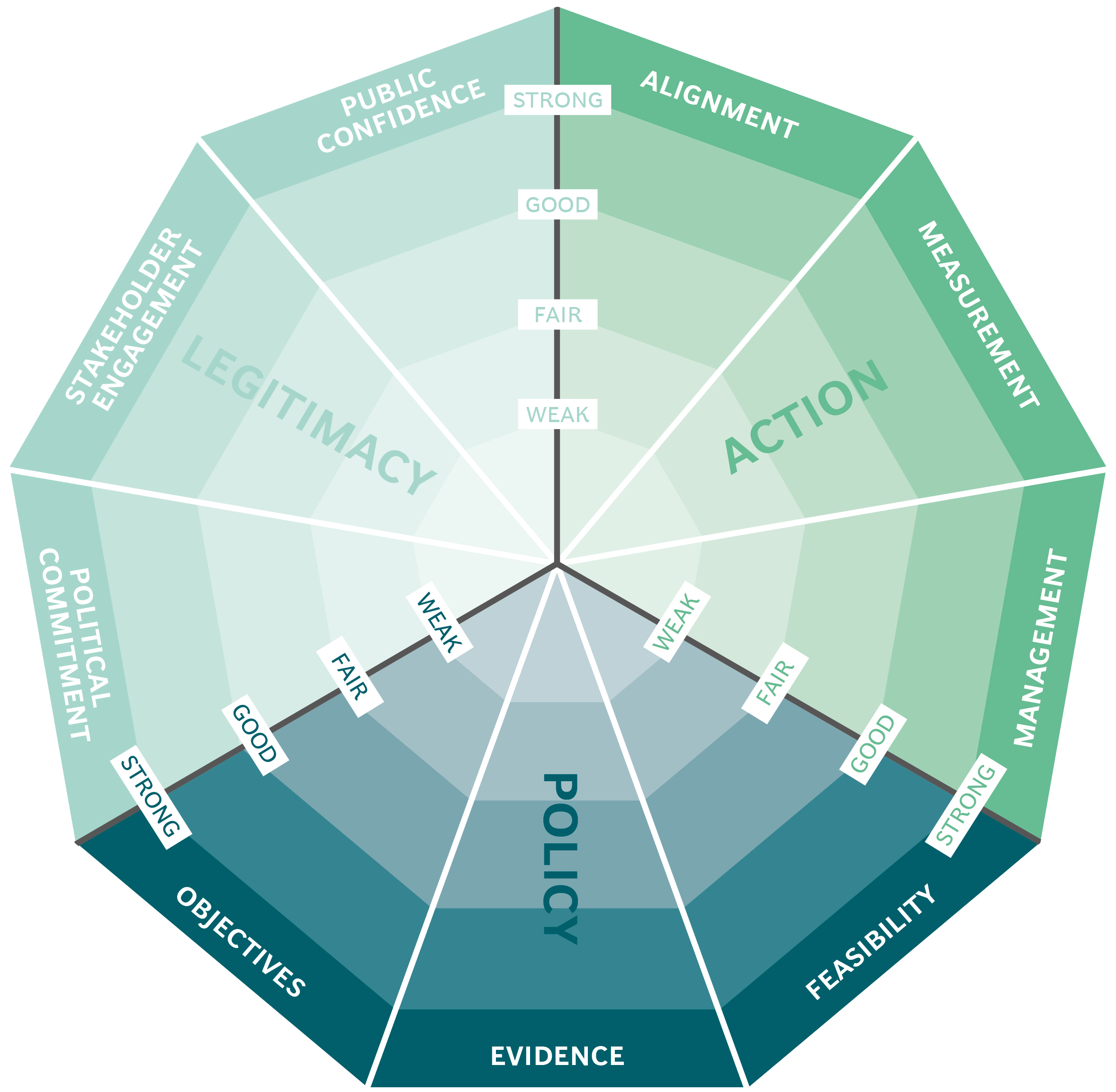
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
