
Crisis resolution and home treatment teams (CRHTTs) in England
The initiative
In 1999, the Department of Health published the National Service Framework for Mental Health (NSF-MH), which set a 10-year agenda for improving mental healthcare for working-age adults in England. It named CRHTTs as the central community-based treatment method.[14] In 2000, the NSF-MH was supported by the NHS Plan and Mental Health Policy Implementation Guide, which mandated the establishment of 335 CRHTTs across England with the objective of providing treatment to 100,000 people annually by 2005.[11][12]. Using calculations based on needs-weighted populations, the Department split these national targets into regional figures for Strategic Health Authorities (SHAs), who in turn developed regional targets for NHS bodies.[11] Each CRHTT was assumed to cover a population of 150,000 and have a caseload of 20 to 30 patients at any one time.[15]
The Implementation Guide included specific information regarding the size of CRHTTs, the actors and institutions they should work with, and the principles and practices they should follow.[15] Policy goals underlying the establishment of CRHTTs included the provision of appropriate and beneficial mental healthcare, the support of earlier discharge from inpatient wards, the reduction of out-of-area treatments (OATs), and the reduction of inpatient admissions and bed occupancy.[11]
CRHTTs provide intensive home treatment for individuals who experience a mental health crisis that would otherwise require hospitalisation.[11] According to the Mental Health Policy Implementation Guide,[16] CRHTTs should act as “gatekeepers” to acute mental health institutions, rapidly assessing individuals with acute mental health problems and referring them to the most appropriate service.[16] They are also required to remain involved until the crisis has been resolved and to ensure that links with appropriate ongoing care services have been made.[15][16]
By offering treatment in private homes, CRHTTs allow patients to be discharged earlier from hospital, while still in the acute phase.[11] Key CRHT features include 24-hour availability and intensive contact in the community, with visits twice daily if needed.[12] CRHTTs are made up chiefly of mental health nurses, with additional input from social workers, consultant psychiatrists, psychologists, and occupational therapists.[11] Although CRHT services are officially aimed at working-age adults (16 to 65), local CRHTTs have the option of deciding to treat patients who fall outside the specified age group.[16] Users of CRHT typically experience challenges such as psychosis, severe depression, or bipolar affective disorder.[11][16]
The 2000 NHS Plan ensured the implementation of CRHTTs throughout England, where only 35 specialist crisis resolution teams existed in just a few regions.[17] LITs were tasked with the establishment of CRHTTs, and they were urged “to reflect, refine and where necessary refocus patterns of treatment and care so as to ensure that any new services are not simply bolted on, but properly and systematically deployed”.[16] LITs included representation from clinicians, other professionals, health and social care managers, the statutory and voluntary sectors, service users, and carers.[16] “Some LITs cover the catchment of a health authority, some of a local authority, and still others of a primary care group, depending on the configuration of local services and the needs of local communities.”[16] The Implementation Guide contains specific information regarding the formation of CRHTTs, including their case load, staffing, and staff training.[16] It also includes very specific implementation steps and targets, the achievement of which has been strongly incentivised through the Care Quality Commission's performance management regulatory regime.[18]
The development of CRHTTs and other initiatives through the NSF-MH required substantial workforce changes. Recognising that new models of care would require workforce diversification and new roles, the Department of Health set up sub-groups on workforce planning in 1999, such as the Workforce Action Team (WAT).[37] [38] The WAT, supported by the National Institute for Mental Health (NIMHE) and its regional centres, has developed a framework of workforce capabilities and created a new staffing role, known as ‘support, time, recovery' (STR) workers.[42] Through these initiatives, NIMHE regional centres, in cooperation with various workforce development confederations, have addressed the issue of recruitment, training, and workforce design in CRHTTs.[42]
The challenge
In the 1990s, it was widely acknowledged that England's long-stay mental health hospitals had to be replaced with more effective community-based alternatives. Yet, public spending on mental health remained low compared with that on physical health,[3] and the government was slow in redirecting budgets from long-stay hospitals to community-based models.[4] A lack of resources complicated the implementation of new treatment methods.[4] The need to promote effective mental health policy and care has long been underlined by statistics pointing to the high number and cost of mental health problems. Each year, around one in four people in the UK experiences challenges to their mental health,[5] which leads to an annual economic and social cost of GBP105 billion in England.[6]
Mental health reforms in 1999 and 2000 continued a long-term deinstitutionalisation process in the UK, which can be traced to the mid-20th century. In the 1950s, existing mental asylums - i.e. long-stay psychiatric hospitals - were publicly criticised for the poor standards of care and quality of life they offered.[7] Socially stigmatised and geographically secluded, asylums provided treatment schemes that violated human rights[7] and were considered iatrogenic (i.e. the treatment itself caused harm).[8][9] It was not until the 1990s that such asylums were closed down, and the first national plans for adult mental health services were created.[10] Policymakers' quest for mental health service plans that were embedded in the community[11] has dominated mental health policy ever since.[9][12]
Reform efforts became more urgent in the late 1990s, when the UK underwent a “crisis in acute care”,[1] marked above all by a shortage in hospital beds - the number of beds per 1,000 of the population had dropped by 40 percent since the late 1970s.[13] Public outcry underscored the need to reduce reliance on “the institutional model” of hospital inpatient care and to implement effective community-based alternatives.
The public impact
Despite a slow start, the number of CRHTTs in England has gradually increased since 2000. Yet, evidence regarding the establishment and effectiveness of CRHT services has been limited and sporadic,[15] making it difficult to assess their impact with any certainty. A striking limitation of the existing research is the lack of description of the variation in case studies and the treatments provided, and the impact of this variation on outcomes.[19]
The variability in the size and function of CRHTTs has made it difficult to assess the impact of this initiative. It is unclear how many CRHTTs are currently operating in England and whether the goal of 335 CRHTTs had been achieved by 2004, though the Department of Health identified 343 CRHTTs in operation in both 2005 and 2007.[11] A national survey conducted in 2018 identified 198 adult Crisis Resolution Teams (a number that excludes other forms of intensive community-based home treatment).[20] Conflicting numbers are often linked to different methods of counting. In some cases, the Department of Health counted very large single teams, serving sizeable populations, as two teams [11]. Controversy also surrounds CRHTTs' performance. Although there were many well-functioning CRHTTs achieving local impact, implementation was variable.[2] In 2005/06, only 40 percent of teams described themselves as fully established according to the Department of Health's guidance. Limited research complicates the assessment of policy goals, especially the reduction in OATs and early discharge from hospital wards.
Because of politicians' interest, the effect of CRHTTs on acute inpatient admission rates constitutes the most widely studied impact.[21] Existing studies have been inconclusive, although initial (government) publications indicated a CRHTT-induced decline in hospital admissions.[19][22] Most of these studies were based on comparisons over time, a method that was later criticised for its lack of scientific robustness. Simple comparisons of areas with CRHTTs before and after policy implementation, or between areas with and without CRHTTs, may overlook the impact of external factors on any changes.[18]
Similarly, a single randomised controlled trial of a CRHT team based in the London Borough of Islington[23] was criticised for lacking applicability to the rest of the country.[18] While evidence shows that, in isolated instances, CRHTTs can reduce hospital admission rates, it does not support any nationwide conclusions. Studies that were published in 2010[24] and 2014[18] argued that the CRHT policy per se has not made a significant difference to admissions.[18] These studies suggest that primary care trusts with already low admission rates were more likely to introduce CRHTTs[18], while declines in admissions were offset by increasing compulsory admissions.[24] With reference to these findings, a national survey published in 2018 described the overall effect of CRHTTs on admission rates as “disappointing”.[20]
Existing research on early discharge and OATs suggests that only 50 percent of CRHTT managers thought effective arrangements were in place to support early discharge from acute wards.[25] In 2016, the Five Year Forward View for Mental Health (FYFV-MH) recommended the development of a first national definition of OATs, later replaced by “Out of Area Placements” (OAPs). [39] Conceptual clarity would then allow for “a new national data collection that will enable accurate measurement and analysis”.[6] The Department of Health directed NHS Digital to introduce and manage a collection of OAP data. Since October 2016, Mental Health Foundation Trusts, Mental Health Non-Foundation Trusts and Independent Sector providers have submitted data to the collection, using the NHS Digital secure online Clinical Audit Platform (CAP).[40]
The impact of CRHTTs on admission rates is closely related to their “gatekeeping” services and 24/7 accessibility.[15] The extent of gatekeeping varied across CRHTTs in England,[25] and several studies suggest that its delivery was limited.[15] A national survey published in 2008 specified that only 68 percent of teams claimed to act as gatekeepers.[2] Similarly, a government-funded study in 2014 found that only 47 percent of Crisis Resolution teams aimed to assess all patients in person before hospital admission. Often assessments involved a single telephone consultation.[25]
It appears that only 40 percent of Crisis Resolution Teams provide a full 24/7 service, while 85 percent provide some around-the-clock “cover”.[25] Their acceptance of referrals also varied: 77 percent were shown to accept referrals from GPs, 55 percent from known service users, and only 20 percent from previously unknown service users.[25] Some but not all CRHTTs accept referrals from housing and emergency services.[25] “CRHTTs vary in how far they provide a multidisciplinary staff team: 90 percent of CRHTTs involved a consultant psychiatrist, 74 percent a social worker, 47 percent an occupational therapist, and 32 percent a psychologist.”[25]
Notwithstanding the government's workforce planning, one negative consequence of the NSF-MH investment has been the exodus of experienced staff from hospitals to community settings.[7] In some cases, new teams were originally set up through internal redeployment, not external recruitment.[41][43] A report by the Sainsbury Centre for Mental Health stated that a quarter of inpatient staff had switched to new community teams. Mental health wards have therefore been left with inexperienced or temporary staff taking care of patients who are very unwell and do not qualify for community-based treatment. Thus, they became increasingly difficult environments for staff to work in and for patients to recover from mental illness.[7][11][46] The NSF-MH has been criticised for failing to prioritize workforce planning.[44] In some areas, the focus on crisis home treatment within CRHTTs was diluted by additional responsibilities, such as the operation of psychiatric liaison services in accident and emergency departments.[25]
Stakeholder engagement
According to NHS sources, the preparation of the NHS Plan involved “specialist teams” of frontline staff, professional groups and patient representatives, as well as senior doctors, nurses and managers. Similarly, the implementation of the NHS Plan (and CRHTTs) involved multiple local stakeholders, who engaged through LITs. LITs typically included health and social care managers and clinicians, along with representatives from statutory and voluntary sectors, professionals, service users, and carers.[16]
The NHS Plan emphasises the goal of combining national policy with regional autonomy, granting discretion to the local stakeholders who were involved in establishing and running CRHTTs. LITs were enabled to refine or refocus patterns of treatment and care in order to ensure that they met local needs and were not simply “bolted on”.[16] In developing a policy understanding of unrecognized local needs, LITs could draw on advice and material provided in the Implementation Guide. [16] Despite its integrative approach, health scientists described the NHS Plan as an “unusually prescriptive attempt to implement a new mental health service model on a national scale”.[20][1] In particular, the matching of resources to need was criticised for being rigid and inflexible,[44] pushing forward service models were rooted “in government policy rather than local enthusiasm or assessment of needs”.[12][45] The National Audit Office found in 2007 that the policy was more focused on outputs (e.g. number of CRHTT treatments) than outcomes (e.g. benefits to patients).[46]
Political commitment
To date, the Department of Health and the NHS, along with other leading institutions in the area of mental health, have endorsed the work of CRHTTs. Implementation of the initial NHS Plan was closely monitored and followed up on. A Mental Health Performance Management Project and a Performance Monitoring Steering Group were established to coordinate and develop national performance monitoring initiatives.[16] According to the 2001 Implementation Guide, they observed the funding and implementation of CRHTTs by each health authority, trust and local authority.[16] In 2004, the Department of Health published The National Service Framework for Mental Health - Five Years On in order to provide a public record of progress against the framework's targets.[17] The Department of Health also continued to trace the number of CRHTTs and the number of home treatment episodes.[26]
In addition, national guidance on mental health service delivery has continued to recommend CRHTTs as a central aspect of acute service pathways in England.[27][28] For example the Mental Health Crisis Care Concordat, a national agreement that was signed in 2014, explicitly highlighted the importance of CRHTTs. Similarly, several government reports have aimed at expanding the CRHT model.[6][29] The government and NHS England has also made explicit attempts to identify and address the shortcomings of CRHTTs, for example by commissioning the FYFV-MH and accepting its recommendations in 2014.
Strong political support for mental health reform and CRHTTs has been reflected in ongoing government and NHS funding. NHS investment has increased every year between 2002 and 2011, rising from GBP38 million to GBP268 million.[12] In the same way, the government continued to fund mental healthcare reforms, pledging GBP1 billion in support of FYFV-MH recommendations in 2016, including GBP400 million for community crisis resolution teams.[6] A press release published at that time announced: “the prime minister pledges a revolution in mental health treatment”.[30]
Public confidence
Public confidence in the NHS, which is in charge of the implementation of CRHTTs, has traditionally been strong in the UK. It also appears that the NHS model for CRHTTs remains broadly supported by stakeholders, although there is limited evidence about the wider public's opinion of CRTTs.[21]
The main institutions in charge of the formal introduction of CRHTTs are the Department of Health and NHS England. Because the interaction with medical staff seems to be a key determinant of patients' trust in healthcare, public perceptions of the NHS are treated as particularly relevant to this assessment of public confidence.[31] The NHS benefits from a long history and has become an integral part of British public consciousness. A 2017 King's Fund study showed that almost four out of five Britons believe that “the NHS is crucial to British society and we must do everything to maintain it”.[32] In 2017, the NHS published the Patient and Public Participation in Commissioning Health and Care Guidance, which sets out benefits, principles and key steps of involving people in health and care. Public engagement initiatives like this are effective attempts in building confidence.[33]
Increasing co-operation between inpatient services and CRHTTs indicates a growing trust and confidence in CRHTTs from the hospital system. Published in 2005, a report by the Sainsbury Centre for Mental Health found that 68 percent of ward managers in England “fully understand the function and remits of community teams”.[43] In 2007, a study conducted on behalf of the National Audit Office observed a shift towards an integrated acute pathway, with CRHTTs moving into close geographic proximity of their respective inpatient unit, sharing buildings and offices. [46] “Some Ward Managers could see the possibility of creating a more attractive acute care career structure through closer merging of ward and CRHT staffing”.[46]
Clarity of objectives
The NHS Plan and its Implementation Guide contained a range of specific numerical targets, including the establishment of 335 CRHTTs, each expected to carry a caseload of 20 to 30 patients at any one time, to see around 300 people a year, and to be available 24/7.[12] The Implementation Guide included a detailed outline of steps involved in setting up CRHTTs and specified their organisational form and tasks, the actors and institutions they should work with, the composition and training of CRHTT staff, and the principles and practices they should follow.[15][16] The NHS Plan and its Implementation Guide are widely considered to be well-defined and specific.[12] The Implementation Guide is updated regularly to incorporate policy lessons.[47][49] For example, the Department issued an updated and clarified Guidance Statement on Fidelity and Best Practice for CRHT in 2007.[48]Strength of evidence
At the time the NHS Plan was devised and implemented, there was relatively little evidence relating to the effectiveness of CRHTTs.[12] While policymakers had worked on the assumption that patients would prefer to be treated at home and that CRHTTs could reduce inpatient beds and costs, their evidence base was limited.[19] Until now, reliable quantitative data has remained in short supply, making it difficult to use practice-based evidence in implementing and improving CRHTTs.[19]
In an attempt to close this data gap, the Department of Health funded the five-year CORE study in 2011. Led by the Camden and Islington NHS Foundation Trust and University College London, it aimed to review and gather evidence about how CRHT services function most effectively.[34] In 2007, the National Audit Office recommended the Department of Health to request regular data collection on CRHT services and user satisfaction from local and national health authorities.[46] While the understanding of best practices is vital to improving the work of CRHTTs, consistent and reliable data on mental healthcare (including CRHTTs) continues to lag behind research in other health areas.[6]
Feasibility
Although the NHS Plan included detailed implementation guidelines and operated within a clearly defined timeframe, its local implementation often suffered from a lack of resources, which negatively impacted the services provided by CRHTTs in England.
The NHS Plan included a specific four-year timeframe for the establishment of 335 CRHTTs. According to government records, the number of CRHTTs reached 343 in 2005, which suggest this timeframe was realistic. The treatment target of 100,000 annually was not met within the given five-year timeframe. In 2004-05, only 69,022 people were treated by CRHTTs.[46] The majority of funding for the NSF-MH and NHS Plan came from central government. Funds included GBP700 million over three years to implement the NSF, and GBP120 million distributed via a Mental Health Modernisation Fund. During implementation (1999/2000 to 2005/06), expenditure on adult mental health services increased by 47 percent, with around a third going into the development of community-based teams.
While budgets were considered in preparing the NHS Plan, research suggests that in some cases allocated resources have been limited, which negatively impacted CRHT services. A National Survey conducted in 2005/06 linked the inadequate implementation of the NHS Plan to a lack of “committed and transparent funding”.[2] Funding for the NSF-MH was often part of already existing unified allocations and extra funding was not always specified.[38] Some local health authorities seemed uncertain about the availability and timing of governmental funding.[38][41] In 2007, the National Audit Office found that CRHT services nationally are resourced at around 90 per cent of the estimated capacity required. However, considerable variation in CRHT staff provision and available resources prevailed at the local level. A report by the Sainsbury Centre for Mental Health in 2004 found that different CRHTTs were funded in different ways and that some struggled securing sufficient resources. The Department of Health gave PCTs discretion to decide how much of their funding was allocated to CRHT services, provided they met their share of national targets. In 2006-07, PCT expenditure on CRHT services ranged from under 1 percent to over 10 percent of their respective mental health budget.[46] In 2007, the National Audit Office found that many CRHTTs could not afford key health and social care professionals, particularly consultant psychiatrists. Hence, their social composition lacked the required skill mix. In 2016, the NHS itself attributed CRHTTs' inability to operate 24/7 to high caseloads and a lack of resources.[35]
Management
The management of the NHS Plan implementation was multi-layered, stretching from the local to the national level. At the national level, the Department of Health and the NHS worked together as “partners”. While the NHS mandated the NHS Plan,[12] it is held accountable by parliament through the secretary of state for health and social care, who acts as its representative.[36] The NIMHE was established in 2001, together with eight regional centres, to oversee the implementation and development of future mental health policy.[38] At a local level, NHS bodies, PCTs, and LITs constituted important managing actors. The establishment of LITs had been a requirement of the NSF-MH, which states that “local health and social care communities must translate the national standards and service models into local delivery plans” and take “ultimate responsibility for ensuring [their] implementation”.[16]
In 2001, there were 126 LITs, which varied in size from region to region. In addition, a range of monitoring bodies were involved in implementing CRHTTs.[16] For example, the Mental Health Taskforce Board was established to oversee the implementation of the NSF-MH and the NHS Plan, and it set up specific taskforce projects. A Mental Health Performance Management Project and a Performance Monitoring Steering Group were established within the context of the NSF-MH to coordinate and develop national performance monitoring initiatives.[16]
The NHS Plan has been praised for its specific and measurable targets and “the degree of performance management associated with its implementation, including nationwide reporting of activity levels and their relationship to centrally set targets”.[12]
Measurement
The Mental Health Performance Assessment Framework constituted an important means of measuring the success of the NHS Plan and the establishment of CRHTTs.[16] It assesses mental health outcomes in terms of mortality (suicide rate reductions), morbidity (reduction in mental illness and improvement in mental health), quality of life for service users and carers, and service user and carer satisfaction.[16] While the development of an assessment framework is useful, it does not measure policy objectives such as the reduction in hospital admissions.
LITs were also required to undertake a self-assessment of progress, in a “traffic light” format, against a total of 35 indicators of the quality of current and planned services as well as the planning process.[16] Due to positive feedback, the Self-Assessment Framework was extended in 2001 and 2002. Its main elements remained constant in order to track progress on key areas over time.[16] Yellow or red light performance led to greater scrutiny, increased funding oversight, and could result in performance management by other agencies. [50]
Alignment
The implementation of the NHS Plan and the subsequent endorsement of the CRHTT model was marked by a close alignment of stakeholders and the broader public. The views of different stakeholder groups do not conflict, although they reflect differences of emphasis: professional stakeholders - ranging from NHS managers to doctors - prioritise organisation and team resources, whereas carers and service users focus on the content and experience of care.[21]
The establishment of CRHTTs has been embedded in a wider socio-political climate that puts mental health on a par with physical health. Mental health problems have become less stigmatised and are increasingly included in community structures. This shift in public awareness benefits the pursuit of community-based mental healthcare models, such as CRHTTs.
Bibliography
[1] Crisis resolution and home treatment in England: where are we now? Sonia Johnson, University College London,
https://www.ucl.ac.uk/core-resource-pack/pdfs/sonia.pdf, Accessed 12 August 2019
[2] Implementation of crisis resolution/home treatment teams in England: national survey 2005-2006, Steve Onyett et al, 2008, Psychiatric Bulletin (2008), 3 2 374-377
https://www.cambridge.org/core/services/aop-cambridge-core/content/view/018666A3226DA198E50DDE6442C5489D/S0955603600037545a.pdf/implementation_of_crisis_resolutionhome_treatment_teams_in_england_national_survey_20052006.pdf, Accessed 12 August 2019
[3] The History of Mental Health Services in Modern England: Practitioner Memories and the Direction of Future Research, John Turner, Rhodri Hayward, Katherine Angel, Bill Fulford, John Hall, Chris Millard and Mathew Thomson, 2015, Medical History, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4595954/, Accessed 12 August 2019
[4] Mental health services in England: The 1990s, Ellen Jane Hollingsworth, 1996, International Journal of Law and Psychiatry, 19 (3-4), 309-325, https://reader.elsevier.com/reader/sd/pii/S0160252796800069?token=CABF96F0D461B699D1A5903CAA83E7F7BEEB7E26DADB65B74F43FD7E36E31E9FDCD292C335F03EDB537C66DD133DAFD9, Accessed 12 August 2019
[5] Mental health policy in England, Elizabeth Parkin, 2018, House of Commons Briefing Paper,
https://researchbriefings.parliament.uk/ResearchBriefing/Summary/CBP-7547#fullreport, Accessed 12 August 2019
[6] The Five Year Forward View for Mental Health, February 2016, Mental Health Taskforce to the NHS,
https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf, Accessed 12 August 2019
[7] From the asylum to community care: learning from experience, Helen Killasby, 2006, British Medical Bulletin,
https://academic.oup.com/bmb/article/79-80/1/245/327153, Accessed 12 August 2019
[8] Mental health history: taking over the asylum, Mark Gould, 2008, HSJ,
https://www.hsj.co.uk/home/mental-health-history-taking-over-the-asylum/1136349.article, Accessed 12 August 2019
[9] Deinstitutionalisation in UK mental health services, Richard Murray et al, 2015, The Health Foundation and The King's Fund, https://www.kingsfund.org.uk/publications/making-change-possible/mental-health-services, Accessed 12 August 2019
[10] Government policy and the National Service Framework for Mental Health: modelling and costing services in England, Jed Boardman and Michael Parsonage, 2009, Advances in psychiatric treatment (2009), vol. 15, 230-240 https://www.cambridge.org/core/services/aop-cambridge-core/content/view/26B358B82C9996D4E3E732FDB987D4ED/S135551460000571Xa.pdf/government_policy_and_the_national_service_framework_for_mental_health_modelling_and_costing_services_in_england.pdf, Accessed 12 August 2019
[11] Helping people through mental health crisis: The role of Crisis Resolution and Home Treatment services, Comptroller and Auditor General, 7 December 2007, National Audit Office,
https://www.nao.org.uk/wp-content/uploads/2007/12/07085.pdf, Accessed 7 August 2019
[12] Crisis resolution and home treatment teams: an evolving model, Sonia Johnson, 2013, University College London,
https://www.cambridge.org/core/services/aop-cambridge core/content/view/5E75A82C58DFF0B41987CE258F638599/S1355514600017235a.pdf/crisis_resolution_and_home_treatment_teams_an_evolving_model.pdf, Accessed 12 August 2019
[13] Peak practice, 7 January 1999, The Economist, https://www.economist.com/britain/1999/01/07/peak-practice, Accessed 12 August 2019
[14] A National Service Framework for Mental Health: Modern Standards & Service Models, September 1999, NHS, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/198051/National_Service_Framework_for_Mental_Health.pdf, Accessed 12 August 2019
[15] Crisis Resolution and Home Treatment: A practical guide, Patrick McGlynn (ed.), 2006, The Sainsbury Centre for Mental Health, https://www.centreformentalhealth.org.uk/sites/default/files/crisis_resolution_and_home_treatment_guide.pdf, Accessed 12 August 2019
[16] The Mental Health Policy Implementation Guide, 2001, Department of Health,
https://webarchive.nationalarchives.gov.uk/20120514200638/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4058960.pdf, Accessed 12 August 2019
[17] The National Service Framework for Mental Health - Five Years On, 2014, Department of Health, https://webarchive.nationalarchives.gov.uk/20130315225112/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4099122.pdf, Accessed 12 August 2019
[18] Impact of crisis resolution and home treatment teams on psychiatric admissions in England, R. Jacobs and E. Barrenho, 2011, The British Journal of Psychiatry,
https://www.cambridge.org/core/services/aop-cambridge-core/content/view/3844FFB76828B0560730EE6940DF3E4F/S0007125000255852a.pdf/impact_of_crisis_resolution_and_home_treatment_teams_on_psychiatric_admissions_in_england.pdf, Accessed 12 August 2019
[19] Crisis resolution teams in the UK and elsewhere, Dienecke Hubeling and Robert Bertram, January 2012,
https://www.tandfonline.com/doi/full/10.3109/09638237.2011.637999, Accessed 12 August 2019
[20] Mental health crisis resolution teams and crisis care systems in England: a national survey, Brynmor Lloyd-Evans, Danielle Lamb, Joseph Barnby, Michelle Eskinazi, Amelia Turner and Sonia Johnson, 2018, The British Journal of Psychiatry (2018) 42, 146-151 https://pdfs.semanticscholar.org/8863/4f012c69ac603e2a38090151d56aa742b2c1.pdf, Accessed 12 August 2019
[21] Implementation of the Crisis Resolution Team model in adult mental health settings: a systematic review, Claire Wheeler, Brynmor Lloyd-Evans, Alasdair Churchard, Caroline Fitzgerald, Kate Fullarton, Liberty Mosse, Bethan Paterson, Clementina Galli Zugaro and Sonia Johnson, 2015, BMC Psychiatry, https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0441-x, Accessed 12 August 2019
[22] Crisis resolution/home treatment teams and psychiatric admission rates in England, Gyles Glover, Gerda Arts and Kannan Suresh Babu, November 2006, The British Journal of Psychiatry, Volume 189, Issue 5
https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/crisis-resolutionhome-treatment-teams-and-psychiatric-admission-rates-in-england/5EF4C35FDA2EC0E3EFF36A3391FB20B7, Accessed 12 August 2019
[23] Outcomes of crises before and after introduction of a crisis resolution team, Sonia Johnson, Fiona Nolan, John Hoult, Ian R. White, Paul Bebbington, Andrew Sandor, Nigel McKenzie, Sejal N. Patel and Stephen Pilling, 2005, The British Journal of Psychiatry, https://www.cambridge.org/core/services/aop-cambridge-core/content/view/4383789A099A0BA96ABB0B3B21F11B69/S0007125000166899a.pdf/outcomes_of_crises_before_and_after_introduction_of_a_crisis_resolution_team.pdf, Accessed 12 August 2019
[24] Controlled comparison of two crisis resolution and home treatment teams, P. Tyrer, F. Gordon, S. Nourmand, M. Lawrence, C. Curran, D. Southgate, B. Oruganti, M. Tyler, S. Tottle, B. North, E. Kulinskaya, J. T. Kaleekal and J. Morgan, 2010, The Psychiatrist,
https://www.i-ht.nl/wp-content/uploads/2014/03/A-controlled-comparison-of-two-crisis-resolution-and-home-treatment-teams.pdf, Accessed 12 August 2019
[25] Crisis Resolution Teams - how are they performing? Brynmor Lloyd-Evans and Sonia Johnson, May, 2014, Mental Health Today
https://www.mentalhealthtoday.co.uk/crisis-resolution-teams-how-are-they-performing, Accessed 12 August 2019
[26] Autumn Performance Report, December 2007, Department of Health,
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/243121/7292.pdf, Accessed 12 August 2019
[27] Psychosis and schizophrenia in adults: Treatment and management, 2014, National Institute for Health and Care Excellence,
http://www.nice.org.uk/Guidance/CG178], Accessed 12 August 2019
[28] Guidance for commissioners of acute care - Inpatient and crisis home treatment, 2013, Joint Commissioning Panel for Mental Health,
http://www.jcpmh.info/good-services/acute-care-services/, Accessed 12 August 2019
[29] Future in mind: Promoting, protecting and improving our children and young people's mental health and wellbeing, April 2013, Department of Health and NHS, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/414024/Childrens_Mental_Health.pdf, Accessed 12 August 2019
[30] Prime Minister pledges a revolution in mental health treatment, January 2016, United Kingdom Government,
https://www.gov.uk/government/news/prime-minister-pledges-a-revolution-in-mental-health-treatment, Accessed 12 August 2019
[31] Public trust in health care: the system or the doctor? M.W. Calnan and E. Sanford, 2004, BMJ Quality & Safety,
https://qualitysafety.bmj.com/content/13/2/92, Accessed 12 August 2019
[32] What does the public think about the NHS? Dan Wellings, September 2017, The Kings Fund,
https://www.kingsfund.org.uk/publications/what-does-public-think-about-nhs, Accessed 12 August 2019
[33] Involving people in health and care guidance, NHS, https://www.england.nhs.uk/participation/involvementguidance/, Accessed 12 August 2019
[34] About the CORE Study, UCL,
https://www.ucl.ac.uk/core-resource-pack/about, Accessed 12 August 2019
[35] Implementing the Five Year Forward View for Mental Health, 18 July 2016, NHS, https://www.england.nhs.uk/wp-content/uploads/2016/07/fyfv-mh.pdf, Accessed 12 August 2019
[36] Framework Agreement between the Department of Health and NHS England, 2014, Department of Health and NHS,
https://www.england.nhs.uk/wp-content/uploads/2014/02/dh-nhse-framewk-agreement.pdf, Accessed 12 August 2019
[37] Mental Health NSF (and the NHS Plan) Workforce Planning, Education and Training Underpinning Programme: Adult Mental Health Services - executive summary of the final report by the Workforce Action Team, 2001, Department of Health,
https://webarchive.nationalarchives.gov.uk/20070403003816/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009624, Accessed 06 September 2019
[38] Case Study 2: The National Service Framework for Mental Health in England, 2015, The Kings Fund,
https://www.kingsfund.org.uk/publications/making-change-possible/national-service-framework-mental-health-england, Accessed 06 September 2019
[39] Out of area placements in mental health services for adults in acute inpatient care, September 2016, Department of Health and Social Care,
https://www.gov.uk/government/publications/oaps-in-mental-health-services-for-adults-in-acute-inpatient-care/out-of-area-placements-in-mental-health-services-for-adults-in-acute-inpatient-care, Accessed 06 September 2019
[40] Out of Area Placements, NHS,
https://digital.nhs.uk/data-and-information/clinical-audits-and-registries/out-of-area-placements-oaps, Accessed 06 September 2019
[41] Transforming Mental Health Care Assertive outreach and crisis resolution in practice, 2004, Anne Chisholm and Richard Ford,
http://intensivehometreatment.com/wp-content/uploads/2010/08/Transforming_Mental_Health_Care.pdf, Accessed 06 September 2019
[42] London's Mental Health Workforce: A review of recent developments, 2002, Leena Genkeer, Pippa Gough and Belinda Finlayson,
https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/london-mental-health-workforce-review-recent-developments-leena-genkeer-pippa-gough-belinda-finlayson-kings-fund-may-2003.pdf, Accessed 06 September 2019
[43] Acute Care 2004: A national survey of adult psychiatric wards in England, 2005, Ines Garcia, Claire Kennett, Mansur Quraishi and Graham Durcan,
https://www.researchgate.net/publication/242558279_Acute_Care_2004_A_national_survey_of_adult_psychiatric_wards_in_England, Accessed 06 September 2019
[44] Implementing mental health policy: learning from previous strategies, 2016, Centre for Mental Health,
https://www.centreformentalhealth.org.uk/sites/default/files/2018-09/implementing_policy.pdf, Accessed 06 September 2019
[45] Transforming mental health services, 2011, The British Journal of Psychiatry,
https://www.cambridge.org/core/services/aop-cambridge-core/content/view/354888B9C0CD241EC234B4E1AAB88837/S0007125000255694a.pdf/transforming_mental_health_services.pdf, Accessed 06 September 2019
[46] Are Crisis Resolution & Home Treatment Services seeing the patients they are
supposed to see?, 2007, The National Audit Office,
https://www.nao.org.uk/wp-content/uploads/2007/12/07085_report_of_interviews.pdf, Accessed 06 September 2019
[47] The NHS Plan: 2 years on, August 2002, The British Journal of Psychiatry,
https://www.cambridge.org/core/journals/psychiatric-bulletin/article/nhs-plan-2-years-on/EFDF855C4FB295040EDFB1ED277A40A9/core-reader, Accessed 06 September 2019
[48] Guidance Statement on Fidelity and Best Practice for Crisis Services, December 2006, NHS, Department of Health and CSIP,
http://intensivehometreatment.com/wp-content/uploads/2012/05/guidance-on-fidelity-for-crisis-services-uk3.pdf, Accessed 06 September 2019
[49] Delivering the government's mental health policies: services, staffing and costs, 2007, Jed Boardman and Michael Parsonage,
https://www.scie-socialcareonline.org.uk/delivering-the-governments-mental-health-policies-services-staffing-and-costs/r/a11G00000017u74IAA, Accessed 06 September 2019
[50] The NHS plan As good as it gets—make the most of it, August 2000, Jennifer Dixon and Steve Dewar, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1118315/, Accessed 06 September 2019
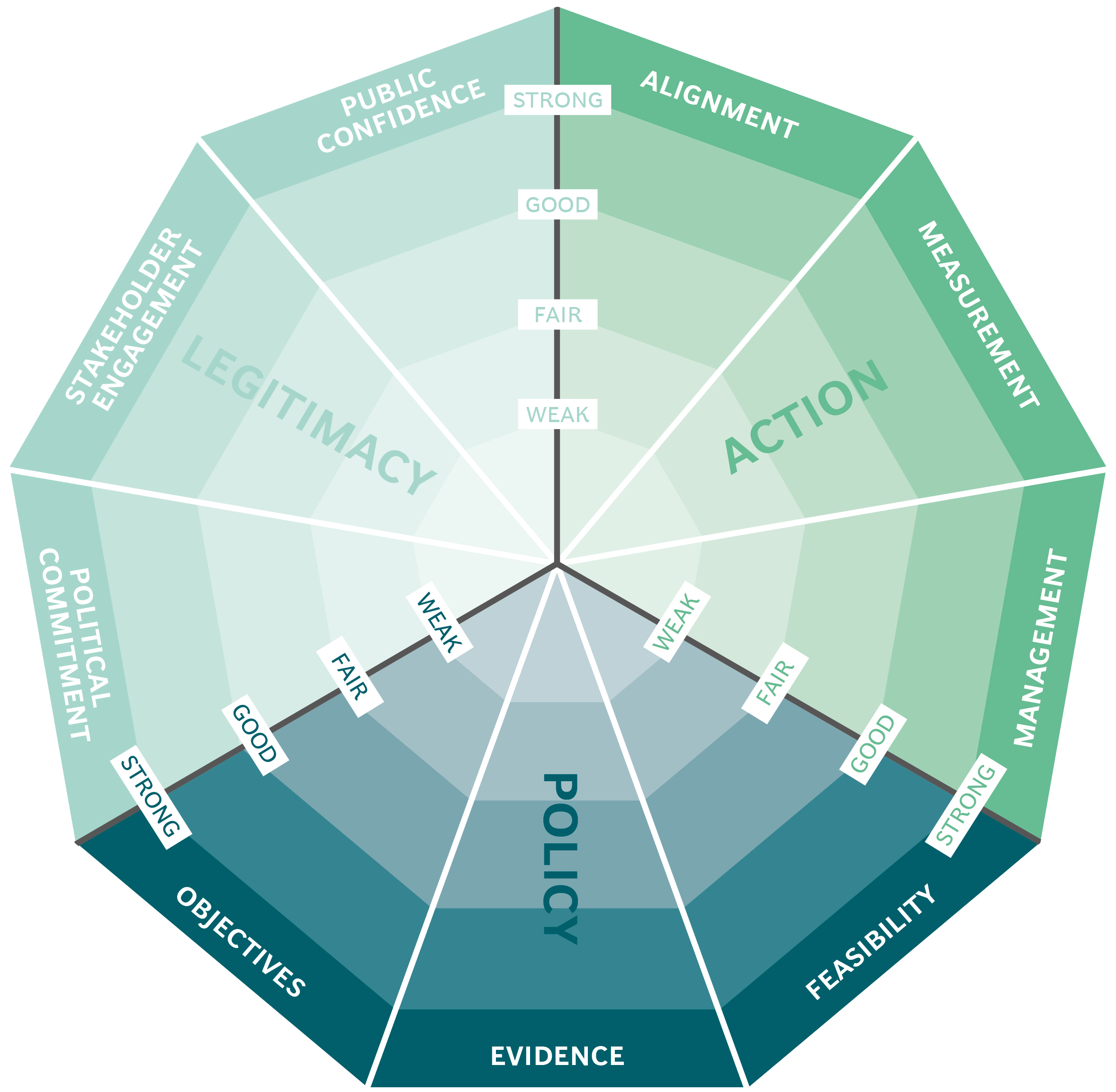
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
